ADVERTISEMENT
Prescribing Orthoses: Has Tissue Stress Theory Supplanted Root Theory?
 Although the biomechanical theories of Merton Root, DPM, have been accepted in academic circles for decades, this author suggests that the principles of tissue stress theory may help inform more effective orthotic prescriptions.
Although the biomechanical theories of Merton Root, DPM, have been accepted in academic circles for decades, this author suggests that the principles of tissue stress theory may help inform more effective orthotic prescriptions.
Custom foot orthoses have been a treatment method for foot and lower extremity pathologies for well over two centuries.
In 1781, Petrus Camper, a Dutch physician, published one of the first books on foot deformities, On the Best Form of Shoe, which stimulated interest in placing arch supporting orthoses into shoes for children’s flatfoot.1 Queen Victoria’s chiropodist, Lewis Durlacher, developed a leather foot orthosis to correct for “plantar pressure lesions” and “foot imbalances” in 1845.2 In 1889, Royal Whitman, MD, developed an orthosis constructed of 18-20 gauge sheet steel made over a plaster cast of a foot in order to raise the medial longitudinal arch of the foot and make it less pronated.3 Edward Reed, MD, an orthopedic surgeon from Santa Monica, Calif., was the first to describe, within the medical literature, plaster splint impression casting for foot orthoses in 1933.4
Then in 1958, Merton Root, DPM, a 1952 graduate from the California College of Chiropody, revolutionized foot orthosis technology by experimenting with new materials called thermoplastics and began developing his Root Functional Orthosis.5 In 1971, Root and colleagues proposed their ideal “eight biophysical criteria for normalcy” and developed a foot and lower extremity classification system that was based on the subtalar joint neutral position.6 They also proposed that all feet and lower extremities that did not meet their criteria for “normal” had structural defects and one should therefore consider these feet “abnormal.”6
In 1971, Root and colleagues also developed the “neutral suspension casting technique” for custom foot orthoses in which they used plaster splints to capture the non-weightbearing contours of the plantar foot while the subtalar joint was in the neutral position and the fourth and fifth metatarsals were dorsiflexed on the rearfoot.7 Finally, in 1977, Root and coworkers published Normal and Abnormal Function of the Foot, their definitive textbook on foot biomechanics and mechanically-based pedal pathologies.8 The book remains an important podiatric textbook to this day.
As a result of his pioneering work in the 1950s, 1960s and 1970s, many consider Root to be the “father of podiatric biomechanics.” Over the past four decades, the ideas and techniques Root proposed have become the best methods by which to evaluate and measure for custom foot orthoses, make impression casts for custom foot orthoses, and design prescription foot orthoses. Until the last two decades, academics were teaching Root’s ideas and techniques as the de facto standard for podiatric biomechanics theory and foot orthosis prescription within the worldwide podiatric profession.
A Closer Look At The Emergence Of Tissue Stress Theory
More recently, however, there has been growing discontent with the biomechanical theories and the orthosis prescription techniques that Root and colleagues first developed over a half-century ago.
In one of the earliest arguments that questioned the validity and wisdom of using the measurement of Root’s “foot deformities” to optimize custom foot orthosis design, Kirby proposed in 1992 that podiatrists should not focus on Root-defined “foot deformities” when designing orthoses for patients.9 He stated that “foot deformity” measurement “does not give us (nearly) enough information to predict the mechanical behavior of the foot and lower extremities during weightbearing activities and, therefore, is insufficient to prescribe the best orthoses for patients.” In addition, he stated that the “magnitude and exact location of pathological tensile, compression or torsional forces on the internal structures are very difficult to predict using the externally measurable parameters such as tibial varum, rearfoot varus, and forefoot to rearfoot relationship.”
 Kirby thought that when prescribing foot orthoses, the podiatrist should be “thinking like an engineer.”9 In other words, he felt that once podiatrists “are certain of the various stresses on the structural components, then we can design our mechanical therapy specifically to reduce or eliminate those stresses” rather than designing foot orthoses to prevent “compensation” for Root-defined “foot deformities.”
Kirby thought that when prescribing foot orthoses, the podiatrist should be “thinking like an engineer.”9 In other words, he felt that once podiatrists “are certain of the various stresses on the structural components, then we can design our mechanical therapy specifically to reduce or eliminate those stresses” rather than designing foot orthoses to prevent “compensation” for Root-defined “foot deformities.”
Three years later, in 1995, McPoil and Hunt also discussed many of the problems they found within the research literature with Root-defined foot biomechanics and foot orthosis theory.10 The authors alternatively proposed using the idea of a “tissue stress model” for prescribing foot orthoses. These authors noted there were problems with the reliability of the measurement techniques that Root advocated and that as a result, Root’s criteria for normal foot alignment were suspect. In addition, they questioned whether the subtalar joint was in the neutral position during walking or not. McPoil and Hunt also noted that using a tissue stress model to prescribe foot orthosis therapy was not a novel idea since the logic of using such an approach was based on the same ideas already currently in use in the treatment of parts of the body other than the foot and ankle.
Furthering the idea of focusing more on internal tissue stress than measuring Root-defined “foot deformities” in 1999, Fuller explained the mechanical significance of the center of pressure relative to the subtalar joint axis.11 In 2000, Fuller discussed how using tissue stress theory could be a tool to better prescribe foot orthoses.12
In 2002, Kirby published three articles that described what he called the “Tissue Stress Approach to Mechanical Foot Therapy.”13 More recently, in 2013, Fuller and Kirby coauthored a mechanical analysis of tissue stress theory.14,15 They explained how one could use subtalar joint axis location and rotational equilibrium theory along with a kinetic analysis of pathological stresses that can occur within the structural components of the foot and lower extremity (i.e. bone, ligament, tendon, muscle, cartilage, fascia and skin) in order to design more effective custom foot orthoses for individuals suffering from mechanically-based pathologies of their feet and lower extremities.
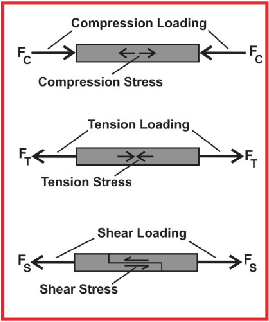 Tissue stress theory relies on the fact that mechanically-based pathologies of the foot and lower extremity all result from pathological magnitudes of stress acting within the structural components of the foot and lower extremity. Stress is an internal measure of how an object resists a loading force and one measures this by dividing the cross-sectional area of that object by the loading force being applied. Stress may be either axial (i.e. compression or tension) or tangential (i.e. shearing) in nature. Compression stress occurs when an object resists being pushed together and tension stress occurs when an object resists being pulled apart. When forces act parallel or tangential to an applied load, one part of an object resists sliding on another part of that object causing a shear stress (see graphic at tleft).
Tissue stress theory relies on the fact that mechanically-based pathologies of the foot and lower extremity all result from pathological magnitudes of stress acting within the structural components of the foot and lower extremity. Stress is an internal measure of how an object resists a loading force and one measures this by dividing the cross-sectional area of that object by the loading force being applied. Stress may be either axial (i.e. compression or tension) or tangential (i.e. shearing) in nature. Compression stress occurs when an object resists being pushed together and tension stress occurs when an object resists being pulled apart. When forces act parallel or tangential to an applied load, one part of an object resists sliding on another part of that object causing a shear stress (see graphic at tleft).
The standard unit of measurement of stress is the pascal (Pa), defined as 1 Newton (N) distributed over 1.0 m2 (1 Pa = 1 N/m2). In scientific studies of tissue mechanics, the megapascal (1 MPa = 1 N/mm2) is the most common unit to measure stress.16
One of the key points in understanding the mechanical nature of tissue injury is that all the body’s tissues exhibit viscoelasticity. Elasticity allows the tissues of the body to return to their original shape once a load is removed. Viscosity causes the tissues of the body to exhibit time-dependent load deformation characteristics that cause strain rate dependency, in which tissues become stiffer the faster they deform.17
In addition, since all the body’s tissues, including bone, are viscoelastic, this means that all the body’s tissues will deform under load with the amount of deformation depending on the magnitude of the loading force. For example, when a ligament has a tension force upon it, it will elongate a small amount under low loads and then return to its original length once that load is removed. However, ligament and tendon will permanently elongate (i.e. undergo plastic deformation) under larger loads and will rupture when under even larger loading forces.
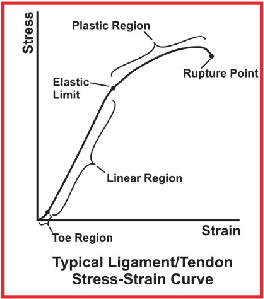 We can quantify the load versus deformation characteristics of all materials, including biological materials, using a stress-strain curve (see the graphic at right). The stress-strain curve of a typical ligament or tendon demonstrates an initial toe region that represents the uncrimping of collagen upon initial loading; a linear region where the ligament or tendon remains elastic and will return to its original shape once the loading force is removed; an elastic limit above the plastic region of the curve where plastic deformation occurs; and a rupture point where the ligament or tendon ruptures.18
We can quantify the load versus deformation characteristics of all materials, including biological materials, using a stress-strain curve (see the graphic at right). The stress-strain curve of a typical ligament or tendon demonstrates an initial toe region that represents the uncrimping of collagen upon initial loading; a linear region where the ligament or tendon remains elastic and will return to its original shape once the loading force is removed; an elastic limit above the plastic region of the curve where plastic deformation occurs; and a rupture point where the ligament or tendon ruptures.18
Therefore, the key to prevention of tissue injury within the foot and lower extremity is to keep the tissues functioning within their elastic range, where tissue loading forces are small enough during their repetitive loading cycles that patients avoid excessive magnitudes of tissue loading forces that may cause plastic deformation of the tissues and tissue injury during weightbearing activities.10,15,19,20
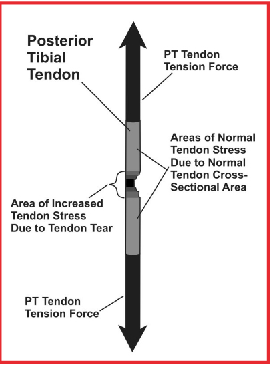 One example of where the structural components of the foot and lower extremity have plastic deformation and cause painful injury includes the elongation and/or rupture of the posterior tibial tendon in posterior tibial tendon dysfunction (PTTD). In this scenario, the tendon tear itself causes even greater magnitudes of stress in the remaining tendon fibers in the region of the tendon tear (see graphic at left). Other examples of plastic deformation of tissues include the disruption of cortical bone in a stress fracture or complete fracture of a metatarsal and the complete rupture of the anterior talofibular ligament in a grade III inversion ankle sprain. In all of these cases, if the stresses acting within the specific structural component of the foot and lower extremity had remained at lower loads, functioning within the elastic range of its stress-strain curve, then plastic deformation and tissue injury would likely not have occurred.
One example of where the structural components of the foot and lower extremity have plastic deformation and cause painful injury includes the elongation and/or rupture of the posterior tibial tendon in posterior tibial tendon dysfunction (PTTD). In this scenario, the tendon tear itself causes even greater magnitudes of stress in the remaining tendon fibers in the region of the tendon tear (see graphic at left). Other examples of plastic deformation of tissues include the disruption of cortical bone in a stress fracture or complete fracture of a metatarsal and the complete rupture of the anterior talofibular ligament in a grade III inversion ankle sprain. In all of these cases, if the stresses acting within the specific structural component of the foot and lower extremity had remained at lower loads, functioning within the elastic range of its stress-strain curve, then plastic deformation and tissue injury would likely not have occurred.
How Tissue Stress Theory Can Guide Orthotic Prescriptions
With these facts of tissue biomechanics in mind, incorporating tissue stress theory into the design of prescription foot orthosis therapy should enable injured tissues to resume function within the elastic region of their stress-strain curve, reducing the risk of further tissue injury and allowing more prompt tissue healing to occur. The three goals of prescription foot orthosis therapy using tissue stress theory are: reducing the pathological loading forces on the injured structural components of the foot and lower extremity; optimizing overall gait function; and preventing other pathologies from occurring.13,15
In the clinical setting, the podiatrist using tissue stress theory needs to utilize the following steps in order to optimize prescription foot orthosis therapy.13,15
First, specifically identify the anatomical structure that is the source of the patient’s complaints. This requires the podiatrist to have a detailed understanding of foot and lower extremity anatomy, a good understanding of clinical tests and access to diagnostic studies that can help identify which structural component is injured.
Second, the podiatrist needs to determine the structural and/or functional variables that may be the source of the pathological forces acting on the injured structure. A complete history, biomechanical examination of the foot and lower extremity, muscle testing, range of motion examination, and gait evaluation may all be necessary to determine what structural and/or functional variables are the main cause or causes of the excessive stress on the injured anatomical structure.
Finally, formulate a therapeutic treatment plan, including specific foot orthosis modifications, shoe modifications, bracing, stretching, strengthening, physical therapy modalities, injection therapy and surgery. One should carry out this plan in a logical sequence in order to optimize patient healing.
Using tissue stress theory to optimize foot orthosis design for patients with mechanically-based foot and lower extremity pathologies requires podiatrists to have a good appreciation of which anatomical structures are subject to tension, compression and shearing stresses during weightbearing activities. In addition, podiatrists must also understand the various ways that they may alter the design of foot orthoses to lessen the magnitude of abnormal stresses acting within the injured tissues of the foot and lower extremity. In other words, the podiatrist must have a good comprehension of the many variables that may mechanically affect the internal loading forces acting on the external and internal structural components of the foot and lower extremity during weightbearing activities.15
Prescribing Orthoses For Specific Injuries
How might one specifically use tissue stress theory versus Root theory to better design an effective foot orthosis for a patient with a foot or lower extremity injury?
In the case of the common injury of proximal plantar fasciitis, the podiatrist must first be aware of the nature of stresses to which the plantar calcaneus is subject during weightbearing activities. The plantar calcaneus is not only subject to tension forces from the pull of the plantar fascia and plantar intrinsic muscles, but is also subject to compression forces from ground reaction force (GRF). Tissue stress theory dictates that, regardless of whether the patient has a Root-defined rearfoot varus or valgus deformity or a forefoot varus or valgus deformity, the pathological stresses causing the plantar calcaneal symptoms will still remain the same.
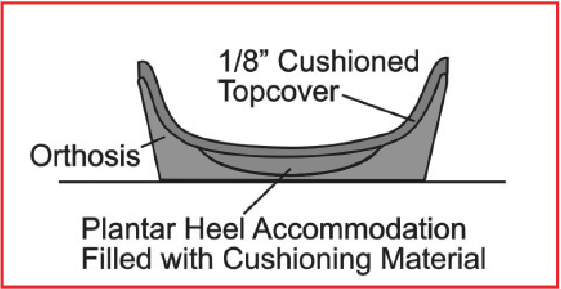 In other words, to treat a patient with proximal plantar fasciitis effectively, the podiatrist doesn’t need to design the prescription foot orthosis using the principles advocated by Root and colleagues. These principles involved “preventing compensation for rearfoot and forefoot deformities,” “causing the subtalar joint (STJ) to function more in the neutral position,” or “locking the midtarsal joint.”13 By using the principles of tissue stress theory, the podiatrist simply needs to design the orthosis to decrease the magnitudes of tension stress and/or compression stress acting on the plantar calcaneus. Possible orthosis modifications may include deep heel cups, well fitting and stiff medial arch contours, padded topcovers and central heel cushioned accommodations within the orthosis heel cup. These modifications should not only reduce the tension stresses acting on the plantar calcaneus from the pull of the plantar fascia and plantar intrinsic muscles, but also reduce the plantar heel compression stresses from ground reaction force acting on the central aspect of the plantar calcaneus (see graphic at right).
In other words, to treat a patient with proximal plantar fasciitis effectively, the podiatrist doesn’t need to design the prescription foot orthosis using the principles advocated by Root and colleagues. These principles involved “preventing compensation for rearfoot and forefoot deformities,” “causing the subtalar joint (STJ) to function more in the neutral position,” or “locking the midtarsal joint.”13 By using the principles of tissue stress theory, the podiatrist simply needs to design the orthosis to decrease the magnitudes of tension stress and/or compression stress acting on the plantar calcaneus. Possible orthosis modifications may include deep heel cups, well fitting and stiff medial arch contours, padded topcovers and central heel cushioned accommodations within the orthosis heel cup. These modifications should not only reduce the tension stresses acting on the plantar calcaneus from the pull of the plantar fascia and plantar intrinsic muscles, but also reduce the plantar heel compression stresses from ground reaction force acting on the central aspect of the plantar calcaneus (see graphic at right).
Using tissue stress theory to optimize foot orthosis design for a patient with posterior tibial tendon dysfunction uses the same biomechanical logic. The first step is to identify the injured tissue as the posterior tibial tendon and next realize that the posterior tibial tendon transmits tension forces from the posterior tibial muscle to the insertions of the posterior tibial tendon. One then needs to design the prescription foot orthosis to reduce the pathological tension stress acting within the posterior tibial tendon, improve gait function of the patient and so other pathologies do not occur.
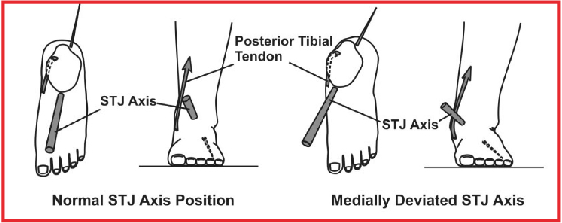 Patients with posterior tibial tendon dysfunction have varying degrees of medial deviation of the subtalar joint axis. Accordingly, ground reaction force acting on the plantar foot will cause excessive magnitudes of subtalar joint pronation moment in these patients and the posterior tibial tendon will also have a reduced subtalar joint axis supination moment arm (see graphic at left). The result is increased posterior tibial muscle contractile activity and increased posterior tibial tension, which is necessary to counterbalance the excessive subtalar joint pronation moments.14,21-24 Prescription foot orthosis modifications such as the medial heel skive, deep heel cup, inverted balancing position, minimal medial arch fill, stiff orthosis plate material and rigid rearfoot posts are required to increase the subtalar joint supination moment from the orthosis. This will subsequently reduce the need for the posterior tibial muscle to be as active, which will in turn decrease the pathological tension stress acting within the posterior tibial tendon.14,24,25
Patients with posterior tibial tendon dysfunction have varying degrees of medial deviation of the subtalar joint axis. Accordingly, ground reaction force acting on the plantar foot will cause excessive magnitudes of subtalar joint pronation moment in these patients and the posterior tibial tendon will also have a reduced subtalar joint axis supination moment arm (see graphic at left). The result is increased posterior tibial muscle contractile activity and increased posterior tibial tension, which is necessary to counterbalance the excessive subtalar joint pronation moments.14,21-24 Prescription foot orthosis modifications such as the medial heel skive, deep heel cup, inverted balancing position, minimal medial arch fill, stiff orthosis plate material and rigid rearfoot posts are required to increase the subtalar joint supination moment from the orthosis. This will subsequently reduce the need for the posterior tibial muscle to be as active, which will in turn decrease the pathological tension stress acting within the posterior tibial tendon.14,24,25
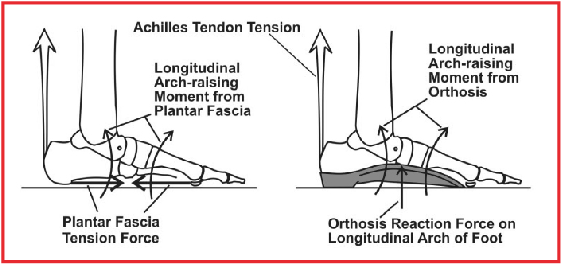 One of the key concepts of tissue stress theory is that in order to best reduce the stress on the injured tissue, one should design the foot orthosis, when possible, to perform the function of the injured tissue during weightbearing activities. For example, in the case of the patient with proximal plantar fasciitis, the plantar fascia causing a longitudinal arch raising moment needs to have its function duplicated by a custom orthosis made with a well-fitting and supportive longitudinal arch. This orthosis will, like the plantar fascia, also cause a longitudinal arch raising moment on the foot (see graphic at right). In other words, the orthosis needs to perform some of the biomechanical functions of the injured tissue in order to most effectively take the stress off that tissue.
One of the key concepts of tissue stress theory is that in order to best reduce the stress on the injured tissue, one should design the foot orthosis, when possible, to perform the function of the injured tissue during weightbearing activities. For example, in the case of the patient with proximal plantar fasciitis, the plantar fascia causing a longitudinal arch raising moment needs to have its function duplicated by a custom orthosis made with a well-fitting and supportive longitudinal arch. This orthosis will, like the plantar fascia, also cause a longitudinal arch raising moment on the foot (see graphic at right). In other words, the orthosis needs to perform some of the biomechanical functions of the injured tissue in order to most effectively take the stress off that tissue.
Likewise, in the case of the patient with posterior tibial tendon dysfunction I have described above, a properly constructed foot orthosis needs to have design features that duplicate the function of the posterior tibial muscle. In other words, one must design the foot orthosis to cause a supination moment across the subtalar joint axis. Using modifications such as a medial heel skive, a well formed arch, a stiff orthosis plate and a rigid rearfoot post, the foot orthosis will cause a subtalar joint supination moment. This moment will, by duplicating the subtalar joint supination moment-producing function of the posterior tibial muscle, reduce the tension stress on the posterior tibial tendon.
In summary, we do not need to design effective foot orthoses to “to prevent compensations for foot deformities” or “to realign the foot toward (subtalar joint) neutral” as Root and colleagues advocated. Instead, we should design orthoses by using tissue stress theory simply to reduce pathological stress on injured tissues.
In Conclusion
The medical professions have used foot orthoses for the treatment of mechanically based foot and lower extremity pathologies for over two centuries. During that time, there have been many important individuals who have influenced foot and lower extremity biomechanics theory and foot orthosis design. One of these individuals, Merton Root, DPM, helped develop the modern thermoplastic foot orthosis and proposed theories on foot and lower extremity function and foot orthosis design. Academics have widely taught these theories within the field of podiatric biomechanics over the last four decades.
However, with the increased knowledge that comes with better research and better biomechanical theory, it is now obvious that many of Dr. Root’s evaluation and treatment methods need refinement, and even replacement, in order to give the best treatment results to our patients. Reevaluating Dr. Root’s methods may also allow podiatrists to stay at the leading edge of prescription foot orthosis theory and practice in the increasingly competitive medical marketplace. Tissue stress theory is currently the best method by which to design prescription foot orthoses for patients with mechanically based foot and lower extremity pathologies. In my opinion, tissue stress theory will eventually supplant the evaluation and treatment techniques advocated by Root and colleagues within the next decade.
Dr. Kirby is an Adjunct Associate Professor within the Department of Applied Biomechanics at the California School of Podiatric Medicine at Samuel Merritt University in Oakland, Calif. He is in private practice in Sacramento, Calif.
References
- Camper P. On the Best Form of Shoe. Translated in: Dowie J. The Foot and Its Covering. Hardwicke, London, 1861.
- Durlacher L. A Concise Treatise on Corns, Bunions, and the Disorders of Nails with Advice for the General Management of the Feet. Simpkin, Marshall and Co, London, 1845.
- Whitman R. Observations of forty-five cases of flat-foot with particular reference to etiology and treatment. Trans Am Orthop Assoc. 1889; 11(1):122-137.
- Reed EN. A simple method for making plaster casts of feet. J Bone Joint Surg. 1933; 17:1007.
- Root ML. How was the Root functional orthotic developed? Podiatry Arts Lab Newsletter, Pekin, Illinois, Fall 1981.
- Root ML, Orien WP, Weed JH, Hughes RJ. Biomechanical Examination of the Foot, Volume 1. Clinical Biomechanics Corporation, Los Angeles, 1971.
- Root ML, Weed JH, Orien WP. Neutral Position Casting Techniques. Clinical Biomechanics Corp., Los Angeles, 1971.
- Root ML, Orien WP, Weed JH. Normal and Abnormal Function of the Foot. Clinical Biomechanics Corp., Los Angeles, CA, 1977.
- Kirby KA. Foot and Lower Extremity Biomechanics: A Ten Year Collection of Precision Intricast Newsletters. Precision Intricast, Inc, Payson, AZ, 1997, pp. 267-268.
- McPoil TG, Hunt GC. Evaluation and management of foot and ankle disorders: Present problems and future directions. JOSPT. 1995; 21(6):381-388.
- Fuller EA. Center of pressure and its theoretical relationship to foot pathology. J Am Podiatr Med Assoc. 1999; 89(6):278-291.
- Fuller EA. Reinventing biomechanics. Podiatry Today. 2000; 13(7):30-36.
- Kirby KA. Foot and Lower Extremity Biomechanics II: Precision Intricast Newsletters, 1997-2002. Precision Intricast, Inc., Payson, AZ, 2002, pp. 11-18.
- Kirby KA. Subtalar joint axis location and rotational equilibrium theory of foot function. J Am Podiatr Med Assoc. 2001; 91(9):465-488.
- Fuller EA, Kirby KA. Subtalar joint equilibrium and tissue stress approach to biomechanical therapy of the foot and lower extremity. In Albert SF, Curran SA (eds): Biomechanics of the Lower Extremity: Theory and Practice, Volume 1. Bipedmed, LLC, Denver, 2013, pp. 205-264.
- Whiting WC, Zernicke RF. Biomechanics of Musculoskeletal Injury, Second Edition. Human Kinetics, Champaign, IL, 2008, p. 81.
- Whiting WC, Zernicke RF. Biomechanics of Musculoskeletal Injury, Second Edition. Human Kinetics, Champaign, IL, 2008, pp. 90-91.
- Whiting WC, Zernicke RF. Biomechanics of Musculoskeletal Injury, Second Edition. Human Kinetics, Champaign, IL, 2008, pp. 83-84.
- Kirby KA. Foot and Lower Extremity Biomechanics III: Precision Intricast Newsletters, 2002-2008. Precision Intricast, Inc., Payson, AZ, 2009, pp. 17-20.
- Kirby KA. Foot and Lower Extremity Biomechanics IV: Precision Intricast Newsletters, 2009-2013. Precision Intricast, Inc., Payson, AZ, 2014, pp. 7-8.
- Kirby KA. Methods for determination of positional variations in the subtalar joint axis. J Am Podiatr Med Assoc. 1987; 77(5):228-234.
- Kirby KA. Rotational equilibrium across the subtalar joint axis. J Am Podiatr Med Assoc. 1989; 79(1):1-14.
- Kirby KA. Biomechanics of the normal and abnormal foot. J Am Podiatr Med Assoc. 2000; 90(1):30-34.
- Kirby KA. Conservative treatment of posterior tibial dysfunction. Podiatry Management. 2000; 19:73-82.
- Kirby KA. The medial heel skive technique: improving pronation control in foot orthoses. J Am Podiatr Med Assoc. 1992; 82(4):177-188.











